What would it take to believe people with pain?
Exploring validation - and invalidation - in the clinical encounter
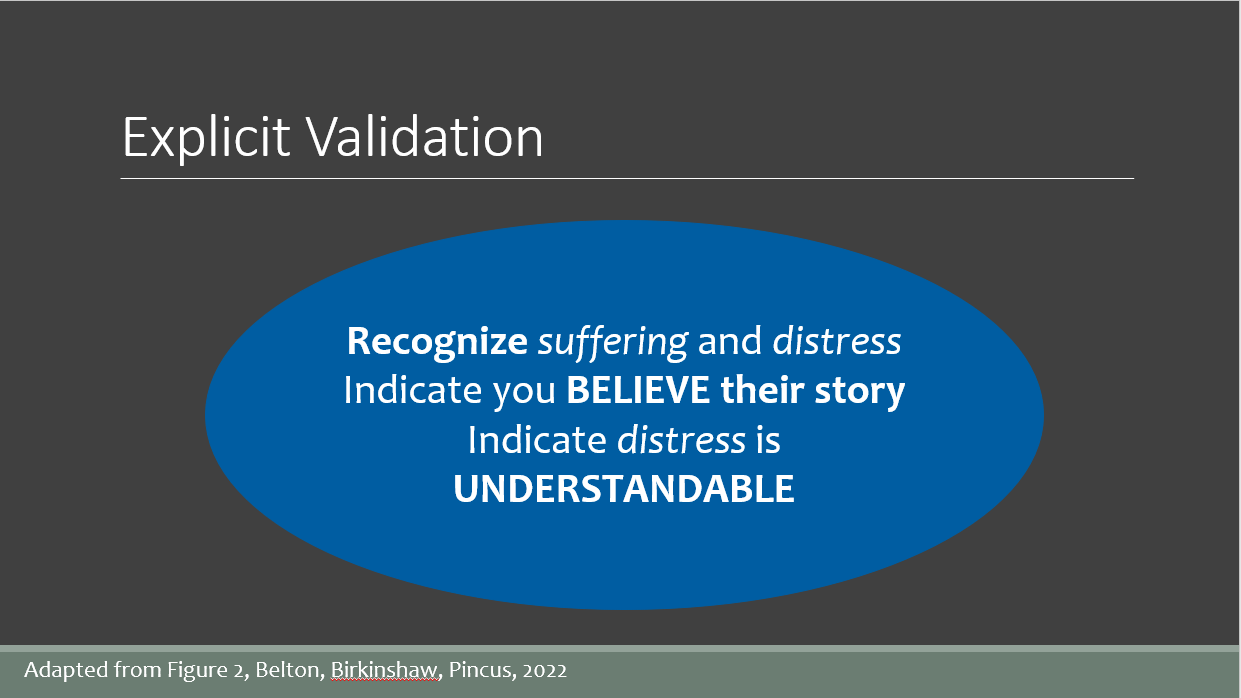
Validation is something that keeps coming up in conversations, on social media, at pain conferences, in my own writing here and in peer-reviewed published articles. But what does validation mean? And why do so many people with pain feel invalidated in their care?
There is push back from some folks when I talk about the importance of validating people and validating their pain. Exploring that push back a bit it seems many of these folks define validation in terms of right and wrong, truth and untruth. That they can’t validate someone’s understanding of their own pain if it’s ‘wrong’ (or unhelpful or maladaptive or whatever) according to what they believe about pain.
Yet that's not what I mean when I use the word validation. Here are some examples of what I personally mean when I talk about validation:
Listening to what I have to say is validating
Believing what I tell you about my experiences is validating
Asking me questions that follow my story is validating
Confirming to me that my pain is real is validating
Acknowledging the impacts of living with pain, that it can really suck, be really challenging, be life- and self-upending, is validating
Acknowledging that my life and self being upended by pain is distressing and really fucking hard is validating
Saying that it absolutely makes sense to believe the things I do about pain and do the things I do because of pain is validating
Eliciting my story, goals, values, dreams, hopes, is validating
Making sense of my pain with me is validating. Bringing together my knowledge and expertise of my pain, life, context with your knowledge and expertise to come up with an explanation that makes biological AND biographical sense, is validating
Co-creating alongside me a path forward that incorporates our shared understanding of what I’m experiencing and my story, goals, values, dreams, and hopes is validating
All of that validation does not mean you have to agree with my explanation for my pain or think I’m doing all the right things for it.

Invalidation
Maybe it's easier to see what validation is, and why I bang on about it, by looking at all of the things that are invalidating (and stigmatizing!) in pain care.
Being told there is nothing ‘really’ wrong with us, that nothing can be found therefore there should be no pain or the pain is ‘unexplainable’.
Being told our pain is all in our head and endless variations on that theme. To paraphrase Sam Bunzli, in the absence of proof of a disordered spine it must be a disordered mind. [Also see Sam’s open acces paper on stigma in low-back pain care)
Being accused of or treated like we are exaggerating, overly emotional, too angry, too reactive, that we’re having ‘outsized responses’ to an injury or illness.
Not being greeted, not making any eye contact, being talked at from behind a computer screen or file.
Being talked over or interrupted.
Being rushed to get to the ‘important stuff’, even though what we are saying is the important stuff that will often lead to a faster and more accurate diagnosis and more relevant therapeutic plan if we are just heard and what we say is considered and explored.
Having our narratives and stories challenged, dismissed, or replaced by a clinical narrative, a science narrative, a medical narrative - the "right" narrative meant to replace our wrong one. This is often an explanatory narrative applicable to everyone, so applies to no one.
Being referred to as non-compliant, challenging, difficult, heartsink, unreliable (she’s an 'unreliable historian'…), unmotivated. If we are still waking up every morning, still seeking care and answers, we are fucking motivated. (Discovering what that motivation is goes a long way toward crafting meaningful therapeutic goals and plans.)
Being just a number, a file, a body part, a problem, a diagnosis. Being referred to by our appointment time, diagnosis, room number, like my "your 2 o'clock hip is here" experience illustrated below by my friend Soula Mantalvanos.
Having to provide objective proof of our pain - an image, a scan, an x-ray, a test, a surgery. It it can be seen our pain is real, if it can’t be seen, it’s evidence that it does not exist (for more, read Pain, objectivity and history: understanding pain stigma by Daniel Goldberg and see Eugenie Lee’s painting If Only and read the accompanying story)
Being accused of malingering (especially in the absence of objective ‘proof’, treated like we are just trying to game ‘the system’, being referred to as seeking ‘secondary gains’ with no recognition of our primary losses and no critical appraisal of how shitty the ‘gains’ really are and how adversarial and harmful and difficult to navigate, let alone ‘game’, the system is (see Ian Harris side note).
(Side note: Ian Harris, author of Surgery, The Ultimate Placebo and, with Rachelle Buchbinder, Hippocrasy: How doctors are betraying their oath, recently presented at the New Zealand Pain Society Annual Meeting. He shared how accident/workers compensation schemes often don’t recognize pain as being legitimate, so claims and care are denied, UNLESS THAT PERSON HAS SURGERY FOR THAT PAIN, then it’s legit. That’s seriously fucked up. Just have back pain? Not legit. Have surgery for that very same back pain? Now the pain is legit! AND you get a percentage of whole person impairment to go with it! When you just had pain, no impairment. But now that you’ve had surgery you are now impaired, thus your pain is legit! What the hell are we doing to people?!?!)
There is too much more I could share, but you get the gist.

Why don’t we believe people in pain?
Why is the healthcare system default to objectify, dehumanize, doubt, and discredit, people with pain?
In my experience the invalidating things happen much more often in pain and health care, for a variety of reasons. We swim in a sea of distrust of patients, perhaps particularly people with pain (stay tuned: a paper will be coming about this soon that I am writing with Ben Darlow! Ben’s 2013 paper on the The Enduring Impact of What Clinicians Say to People With Low Back Pain had a huge impact on me back when I was first trying to make sense of my own pain and care).
At the San Diego Pain Summit last month (sadly the last, more on that later, but you can find lots of wonderful talks from over the years on the SDPS YouTube page), an attendee who teaches DPT (Doctorate of Physical Therapy) students reflected that students come in bursting with humanity and wanting to make a difference, and we teach their humanity right out of them before they graduate and start seeing patients.
We do this through teaching a very biomedical model, where ‘objectivity’ reigns supreme and RCTs and meta-analyses rule. We teach them that as clinicians they should not bring their human selves to the clinical encounter. That subjectivity is bad. We teach them that people are trying to game the system, that they’re out for secondary gains, that they are malingers who have to be rooted out so those who are actually worthy can receive care.
Where this leads…
When our pain experiences - our human experiences - do not fit into this biomedical narrative, when there is no ‘objective’ proof of pain, or the ‘evidence’ is uncertain, what happens?
What happens when we do not value the knowledge and expertise that people bring to the encounter about their pain, their selves, their lives? When we do not value our own knowledge about what it means to be in pain, to be human, to seek care?
When an experience does not fit into a biomedical box, does not fit into what we’ve been taught to value, does not match our own experiences, we simply just don’t believe it. We begin from a place of distrust. A place of invalidation.
It’s a shitty place to be, that place of invalidation. None of us want to be there. And the reality is that all of us are likely to be patients some day, or someone we love will be a patient. And these invalidating examples will make up some part of our experience in the healthcare system. Whether that part is large or small depends on a lot of factors that I’ve explored elsewhere, but even the most privileged among us often have a shitty time of it.
That’s messed up.
How did we get here? How do we get outta here? It’s not a bunch of bad actors treating people poorly that we need to get rid of somehow. We’re all swimming in this sea of distrust, born (at least in part) of a need to objectify and prove human experiences of pain and suffering. We all play a role in maintaining the status quo.

Challenging and changing the status quo
At the recent NZPS Annual Meeting I critiqued the evidence hierarchy and evidence-based medicine in one of my presentations. I was approached afterward and warned/told not to do so so strongly (very nicely by a nice person, but still), because EBM started from a place of protecting patients from snake-oil salesmen and the like. I don’t know about that. I’m sure we could interrogate the motivations a bit and find it wasn’t so altruistic after all.
Even if it was all about the patients (but could it be, really, when it didn’t even include them in the process?), shouldn’t we then be alarmed and angry about how EBM has been used against patients? How it’s been used to deny their experiences, their humanity, their trustworthiness, their worth? And thus used to deny them compassion and treatment and care? Shouldn’t that be a reason to challenge it, interrogate the roots of the problems, make it better?
The status quo isn’t just harmful for patients, it’s harmful for clinicians, for health professionals, for researchers, for academics, for policymakers, for educators, for society, for all of us. We are all humans, after all.
We all operate within these shitty systems. And, for far too long, too many of us have upheld them, like the man so worried about me challenging EBM from my small stage.
We don’t have to keep doing things the way they’ve always been done
We can be more reflective, more challenging, more inquisitive about why we believe the things we believe, how we know the things we know, why we do the things we do.
We can change things. We can change the shitty system. Especially if we come together to do so.
I’ve already written more than I intended, and there will surely be more to come, but I’ll leave you with couple questions I’d love to discuss in the comments:
What would happen if we started from a place of believing people when they say they have pain? What if we started from a place of validating their experiences? Their humanity?
What would it take to just believe people with pain?
As always, thanks for being here.







You made it to our Cedar Grove! My Mum will be thrilled. Thanks for making the trip all the way down South.
Whenever I (as a General Practitioner, Pain Doctor and researcher) am giving a teaching session about pain, I always begin by asking people to define "pain". After discussing a few approaches to such a definition, I then present two on a slide: (1) the IASP definition (which I think is good); and (2) "pain is what the person says it is." In fact, the latter is almost a cliché, in my experience, and has always been received positively. So that makes me wonder how we got from that understanding to the point that you're describing in your excellent article - a point which I fully recognise, and do my best to address in my own practice. Thank you.